

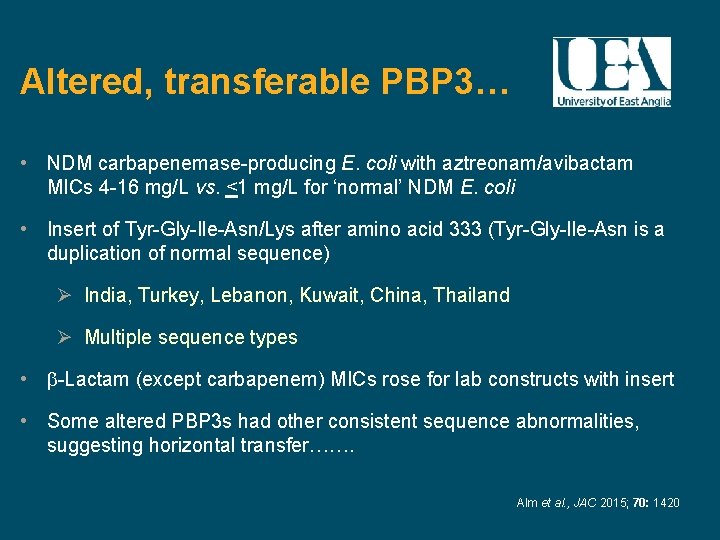
Antibiotic resistance is not limited to human medicine, a similar trend has been found in the veterinary field because equivalent quantities of antibiotics are inadequately used in livestock to improve the health and production of animals, even resistance has been reported from organic farms. According to the Global Risk report of the World Economic Forum, antibiotic resistance is one of the worst universal risks to animal and human health. Infections due to multidrug-resistant (MDR) bacteria are increasing worldwide, and the number of untreatable diseases is rapidly growing. By keeping in view, the molecular ways of resistance development, multifactorial and coordinated measures may be taken to counter the challenge of rapidly increasing β-lactam resistance. The present review article provides information on the recent findings regarding the molecular mechanisms of resistance to β-lactams in Gram-negative bacteria, including CTX-M-type ESBLs with methylase activity, plasmids harbouring phages with β-lactam resistance genes, the co-presence of β-lactam resistant genes of unique combinations and the presence of β-lactam and non-β-lactam antibiotic-resistant genes in the same bacteria. Over time, these new molecular-based resistance mechanisms have been progressively disclosed. Resistance due to β-lactamases develops through to a variety of mechanisms, and the number of resistant genes is involved that can be transferred between bacteria, mostly via plasmids. Therefore, it is imperative to present a comprehensive review of the mechanisms responsible for the development of antimicrobial resistance. β-lactamases constitute a paradigm shift in the evolution of antibiotic resistance. The most harmful of the resistant bacteria are β-lactamases producing Gram-negative species (β-lactamases). Antibiotic-resistant bacteria are considered one of the major global threats to human and animal health.


 0 kommentar(er)
0 kommentar(er)
